Cholesterol is a waxy substance that's found in the fats (lipids) in your blood. While your body needs cholesterol to continue building healthy cells, having high cholesterol can increase your risk of heart disease.
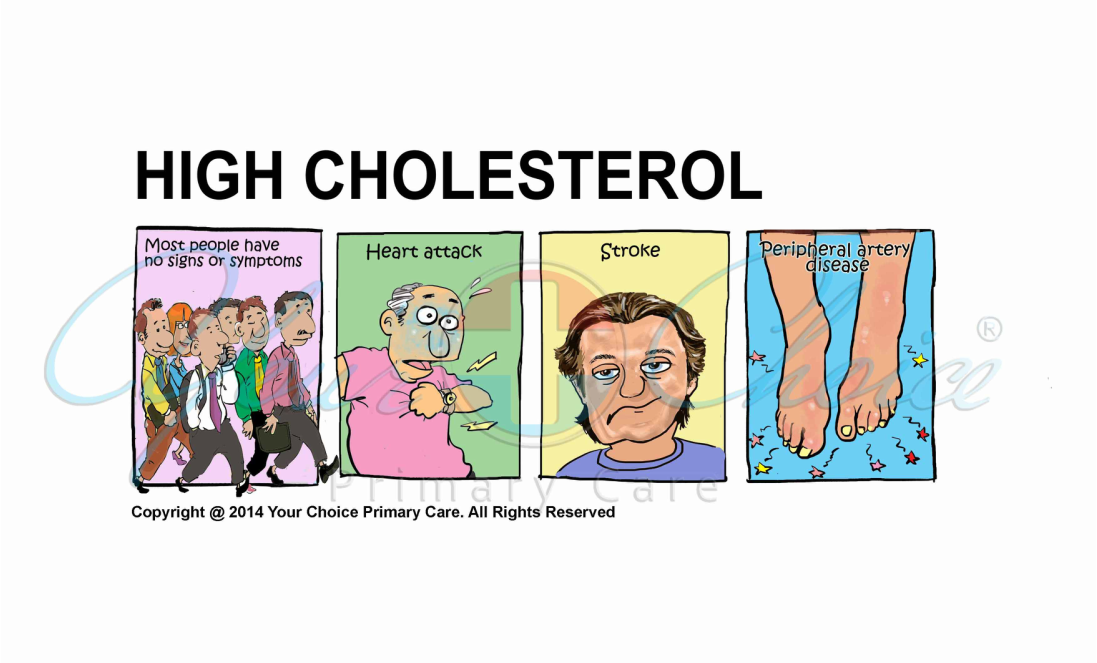
When you have high cholesterol, you may develop fatty deposits in your blood vessels. Eventually, these deposits make it difficult for enough blood to flow through your arteries. Your heart may not get as much oxygen-rich blood as it needs, which increases the risk of a heart attack. Decreased blood flow to your brain can cause a stroke.
High cholesterol (hypercholesterolemia) can be inherited, but it's often the result of unhealthy lifestyle choices, and thus preventable and treatable. A healthy diet, regular exercise and sometimes medication can go a long way toward reducing high cholesterol.
High cholesterol has no symptoms until it’s too late. A blood test is the only way to detect high cholesterol.
When to see a doctor
Ask your doctor for a baseline cholesterol test at age 20 and then have your cholesterol retested once a year.
If your test results aren't within desirable ranges, your doctor may recommend more frequent measurements. Your doctor may also suggest you have more frequent tests if you have a family history of high cholesterol, heart disease or other risk factors, such as smoking, diabetes or high blood pressure.
Cholesterol is carried through your blood, attached to proteins. This combination of proteins and cholesterol is called a lipoprotein. You may have heard of different types of cholesterol, based on what type of cholesterol the lipoprotein carries. They are:
- Low-density lipoprotein (LDL). LDL, or "bad," cholesterol transports cholesterol particles throughout your body. LDL cholesterol builds up in the walls of your arteries, making them hard and narrow.
- Very-low-density lipoprotein (VLDL). This type of lipoprotein contains the most triglycerides, a type of fat, attached to the proteins in your blood. VLDL cholesterol makes LDL cholesterol larger in size, causing your blood vessels to narrow. If you're taking cholesterol-lowering medication but have a high VLDL level, you may need additional medication to lower your triglycerides.
- High-density lipoprotein (HDL). HDL, or "good," cholesterol picks up excess cholesterol and takes it back to your liver.
You're more likely to have high cholesterol that can lead to heart disease if you have any of these risk factors:
- Smoking. Cigarette smoking damages the walls of your blood vessels, making them likely to accumulate fatty deposits. Smoking may also lower your level of HDL, or "good," cholesterol.
- Obesity. Having a body mass index (BMI) of 30 or greater puts you at risk of high cholesterol.
- Large waist circumference. Your risk increases if you are a man with a waist circumference of at least 40 inches (102 centimeters) or a woman with a waist circumference of at least 35 inches (89 centimeters).
- Poor diet. Foods that are high in cholesterol, such as red meat and full-fat dairy products, will increase your total cholesterol. Eating saturated fat, found in animal products, and trans fats, found in some commercially baked cookies and crackers, also can raise your cholesterol level.
- Lack of exercise. Exercise helps boost your body's HDL "good" cholesterol while lowering your LDL "bad" cholesterol. Not getting enough exercise puts you at risk of high cholesterol.
- Diabetes. High blood sugar contributes to higher LDL cholesterol and lower HDL cholesterol. High blood sugar also damages the lining of your arteries.
- Chest pain. If the arteries that supply your heart with blood (coronary arteries) are affected, you may have chest pain (angina) and other symptoms of coronary artery disease.
- Heart attack. If plaques tear or rupture, a blood clot may form at the plaque-rupture site — blocking the flow of blood or breaking free and plugging an artery downstream. If blood flow to part of your heart stops, you'll have a heart attack.
- Stroke. Similar to a heart attack, if blood flow to part of your brain is blocked by a blood clot, a stroke occurs.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet. For a cholesterol test, you will likely have to avoid eating or drinking anything (other than water) for nine to 12 hours before the blood sample is taken.
- Write down key personal information, including a family history of high cholesterol, heart disease, stroke, high blood pressure or diabetes, and any major stresses or recent life changes, as well as exposure to other cardiac risks, such as a personal history of smoking or exposure to family members who smoke (secondary exposure).
- Make a list of all medications, as well as any vitamins or supplements, that you're taking.
- Take a family member or friend along, if possible. Sometimes it can be difficult to soak up all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Be prepared to discuss your diet and exercise habits. If you don't already exercise or eat a healthy diet, be ready to talk to your doctor about any challenges you might face in getting started.
A blood test to check cholesterol levels — called a lipid panel or lipid profile — typically reports:
- Total cholesterol
- LDL cholesterol
- HDL cholesterol
- Triglycerides — a type of fat in the blood
The American Heart Association (AHA) recommends that a triglyceride level of 100 mg/dL (1.3 mmol/L) or lower is considered "optimal." The AHA says this optimal level would improve your heart health. For those trying to lower their triglycerides to this level, lifestyle changes such as diet, weight loss and physical activity are encouraged. That's because triglycerides usually respond well to dietary and lifestyle changes.
Because LDL cholesterol is a major risk factor for heart disease, it's the main focus of cholesterol-lowering treatment. Your target LDL number can vary, depending on your underlying risk of heart disease.
Most people should aim for an LDL level below at least 130 mg/dL (3.4 mmol/L). If you have other risk factors for heart disease, your target LDL should be below 100 mg/dL (2.6 mmol/L). If you're at very high risk of heart disease, you will need to aim for an LDL level below 70 mg/dL (1.8 mmol/L). In general, the lower your LDL cholesterol level is, the better.
You're considered to be at a high risk of heart disease if you:
- Have had a previous heart attack or stroke
- Have artery blockages in your neck (carotid artery disease)
- Have artery blockages in your arms or legs (peripheral artery disease)
- Have known diabetes that requires treatment
- Smoking
- High blood pressure
- Low HDL cholesterol
- Family history of early heart disease
- Age older than 45 if you're a man, or older than 55 if you're a woman
- Elevated lipoprotein (a), another type of fat (lipid) in your blood
The specific choice of medication or combination of medications depends on various factors, including your individual risk factors, your age, your current health and possible side effects. Common choices include:
- Statins. Statins — among the most commonly prescribed medications for lowering cholesterol — block a substance your liver needs to make cholesterol. This causes your liver to remove cholesterol from your blood. Statins may also help your body reabsorb cholesterol from built-up deposits on your artery walls, potentially reversing coronary artery disease. Choices include atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Altoprev, Mevacor), pitavastatin (Livalo), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor).
- Bile-acid-binding resins. Your liver uses cholesterol to make bile acids, a substance needed for digestion. The medications cholestyramine (Prevalite), colesevelam (Welchol) and colestipol (Colestid) lower cholesterol indirectly by binding to bile acids. This prompts your liver to use excess cholesterol to make more bile acids, which reduces the level of cholesterol in your blood.
- Cholesterol absorption inhibitors. Your small intestine absorbs the cholesterol from your diet and releases it into your bloodstream. The drug ezetimibe (Zetia) helps reduce blood cholesterol by limiting the absorption of dietary cholesterol. Zetia can be used in combination with any of the statin drugs.
- Combination cholesterol absorption inhibitor and statin. The combination drug ezetimibe-simvastatin (Vytorin) decreases both absorption of dietary cholesterol in your small intestine and production of cholesterol in your liver.
If you also have high triglycerides, your doctor may prescribe:
- Fibrates. The medications fenofibrate (TriCor) and gemfibrozil (Lopid) decrease triglycerides by reducing your liver's production of very-low-density lipoprotein (VLDL) cholesterol and by speeding up the removal of triglycerides from your blood. VLDL cholesterol contains mostly triglycerides.
- Niacin. Niacin (Niaspan) decreases triglycerides by limiting your liver's ability to produce LDL and VLDL cholesterol.
- Omega-3 fatty acid supplements. Omega-3 fatty acid supplements can help lower your cholesterol. You can take over-the-counter supplements, or your doctor may prescribe Lovaza, a prescription omega-3 fatty acid supplement, as a way to lower your triglycerides. These supplements may be taken with another cholesterol-lowering medication, such as a statin. If you choose to take over-the-counter supplements, get your doctor's OK first.
Tolerance of medications varies from person to person. The common side effects are muscle pains, stomach pain, constipation, nausea and diarrhea. If you decide to take cholesterol medication, your doctor may recommend liver function tests to monitor the medication's effect on your liver.
Excess weight contributes to high cholesterol. Losing even 5 to 10 pounds can help lower total cholesterol levels. Start by taking an honest look at your eating habits and daily routine. Consider your challenges to weight loss — and ways to overcome them. Set long-term, sustainable goals.
Eat heart-healthy foods
What you eat has a direct impact on your cholesterol level. In fact, a diet rich in fiber and other cholesterol-lowering foods may help lower cholesterol as much as statin medication for some people.
- Choose healthier fats. Saturated fat and trans fat raise your total cholesterol and LDL cholesterol. Get no more than 10 percent of your daily calories from saturated fat. Monounsaturated fat — found in olive, peanut and canola oils — is a healthier option. Almonds and walnuts are other sources of healthy fat.
- Eliminate trans fats. Trans fats, which are often found in margarines and commercially baked cookies, crackers and snack cakes, are particularly bad for your cholesterol levels. Not only do trans fats increase your total LDL ("bad") cholesterol, but they also lower your HDL ("good") cholesterol.
- You may have noticed more food labels now market their products as "trans fat-free." But don't rely only on this label. In the United States, if a food contains less than 0.5 grams of trans fat a serving, it can be marked trans fat-free. It may not seem like much, but if you eat a lot of foods with a small amount of trans fat, it can add up quickly. Instead, read the ingredients list. If a food contains a partially hydrogenated oil, that's a trans fat, and you should look for an alternative.
- Limit your dietary cholesterol. Aim for no more than 300 milligrams (mg) of cholesterol a day — or less than 200 mg if you have heart disease. The most concentrated sources of cholesterol include organ meats, egg yolks and whole milk products. Use lean cuts of meat, egg substitutes and skim milk instead.
- Select whole grains. Various nutrients found in whole grains promote heart health. Choose whole-grain breads, whole-wheat pasta, whole-wheat flour and brown rice. Oatmeal and oat bran are other good choices.
- Stock up on fruits and vegetables. Fruits and vegetables are rich in dietary fiber, which can help lower cholesterol. Snack on seasonal fruits. Experiment with vegetable-based casseroles, soups and stir-fries.
- Eat heart-healthy fish. Some types of fish — such as cod, tuna and halibut — have less total fat, saturated fat and cholesterol than do meat and poultry. Salmon, mackerel and herring are rich in omega-3 fatty acids, which help promote heart health.
- Drink alcohol only in moderation. Moderate use of alcohol may increase your levels of HDL cholesterol — but the benefits aren't strong enough to recommend alcohol for anyone who doesn't drink already. If you choose to drink, do so in moderation. This means no more than one drink a day for women and one to two drinks a day for men.
Regular exercise can help improve your cholesterol levels. With your doctor's OK, work up to 30 to 60 minutes of exercise a day. Take a brisk daily walk. Ride your bike. Swim laps. To maintain your motivation, keep it fun. Find an exercise buddy or join an exercise group. And, you don't need to get all 30 to 60 minutes in one exercise session. If you can squeeze in three to six 10-minute intervals of exercise, you'll still get some cholesterol-lowering benefits.
Don't smoke
If you smoke, stop. Quitting can improve your HDL cholesterol level. And the benefits don't end there. Just 20 minutes after quitting, your blood pressure decreases. Within 24 hours, your risk of a heart attack decreases. Within one year, your risk of heart disease is half that of a smoker's. Within 15 years, your risk of heart disease is similar to that of someone who's never smoked.
Few natural products have been proven to reduce cholesterol, but some might be helpful. With your doctor's OK, consider these cholesterol-lowering supplements and products:
- Artichoke
- Barley
- Beta-sitosterol (found in oral supplements and some margarines, such as Promise Activ)
- Blond psyllium (found in seed husk and products such as Metamucil)
- Garlic
- Oat bran (found in oatmeal and whole oats)
If you choose to take cholesterol-lowering supplements, remember the importance of a healthy lifestyle. If your doctor prescribes medication to reduce your cholesterol, take it as directed.
The same heart-healthy lifestyle changes that can lower your cholesterol can help prevent you from having high cholesterol in the first place. To help prevent high cholesterol, you can:
- Lose extra pounds and maintain a healthy weight
- Quit smoking
- Eat a low-fat, low-salt diet that includes many fruits, vegetables and whole grains
- Exercise on most days of the week for at least 30 minutes
- Drink alcohol in moderation, if at all