Allergies occur when your immune system reacts to a foreign substance — such as pollen, bee venom or pet dander — that doesn't cause a reaction in most people.
Your immune system produces substances known as antibodies. Some antibodies protect you from unwanted invaders that could make you sick or cause infection.
When you have allergies, your immune system makes antibodies that identify a particular allergen as harmful, even though it isn't. When you come into contact with the allergen, your immune system's reaction can inflame your skin, sinuses, airways or digestive system.
The severity of allergies varies from person to person and can range from minor irritation to anaphylaxis — a potentially life-threatening emergency.
Allergy symptoms depend on the substance involved and can involve the airways, sinuses and nasal passages, skin, and digestive system. Allergic reactions can range from mild to severe. In some severe cases, allergies can trigger a life-threatening reaction known as anaphylaxis.
Hay fever, also called allergic rhinitis, may cause:
- Sneezing
- Itching of the nose, eyes or roof of the mouth
- Runny, stuffy nose
- Watery, red or swollen eyes (conjunctivitis)
- Tingling mouth
- Swelling of the lips, tongue, face or throat
- Hives
- Anaphylaxis
- A large area of swelling (edema) at the sting site
- Itching or hives all over your body
- Cough, chest tightness, wheezing or shortness of breath
- Anaphylaxis
- Hives
- Itchy skin
- Rash
- Facial swelling
- Wheezing
- Anaphylaxis
- Itch
- Redden
- Flake or peel
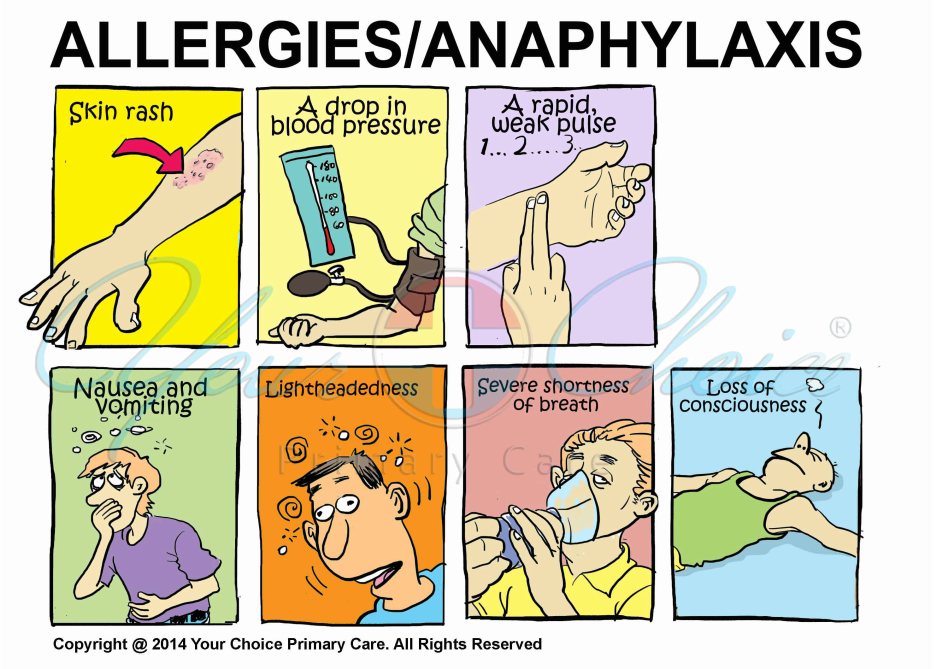
Some types of allergies, including allergies to foods and insect stings, have the potential to trigger a severe reaction known as anaphylaxis. A life-threatening medical emergency, this reaction can cause you to go into shock. Signs and symptoms of anaphylaxis include:
- Loss of consciousness
- A drop in blood pressure
- Severe shortness of breath
- Skin rash
- Lightheadedness
- A rapid, weak pulse
- Nausea and vomiting
When to see a doctor
You might see a doctor if you have symptoms you think may be caused by an allergy, especially if you notice something that seems to trigger your allergies.
For a severe allergic reaction (anaphylaxis), call 911 or your local emergency number.
If you carry an epinephrine auto-injector (such as EpiPen, Auvi-Q, others), give yourself a shot right away.
Even if symptoms improve after an epinephrine injection, a visit to the emergency department is still necessary to make sure symptoms don't return when the effects of the injection wear off.
If you've had a severe allergy attack or any signs and symptoms of anaphylaxis in the past, make an appointment to see your primary care doctor. Evaluation, diagnosis and long-term management of anaphylaxis are complicated, so you'll probably need to see a doctor who specializes in allergies and immunology.
An allergy starts when your immune system mistakes a normally harmless substance for a dangerous invader. The immune system then produces antibodies that remain on the alert for that particular allergen. When you're exposed to the allergen again, these antibodies can release a number of immune system chemicals, such as histamine, that cause allergy symptoms.
Common allergy triggers include:
- Airborne allergens, such as pollen, animal dander, dust mites and mold
- Certain foods, particularly peanuts, tree nuts, wheat, soy, fish, shellfish, eggs and milk
- Insect stings, such as bee stings or wasp stings
- Medications, particularly penicillin or penicillin-based antibiotics
- Latex or other substances you touch, which can cause allergic skin reactions
- Have a family history of asthma or allergies. You're at increased risk of allergies if you have family members with asthma or allergies such as hay fever, hives or eczema.
- Are a child. Children are more likely to develop an allergy than are adults. Children sometimes outgrow allergic conditions as they get older. However, it's not uncommon for allergies to go away and then come back some time later.
- Have asthma or an allergic condition. Having asthma increases your risk of developing an allergy. Also, having one type of allergic condition makes you more likely to be allergic to something else.
- Anaphylaxis. If you have severe allergies, you're at increased risk of this serious allergy-induced reaction. Anaphylaxis is most commonly associated with food allergy, penicillin allergy and allergy to insect venom.
- Asthma. If you have an allergy, you're more likely to have asthma — an immune system reaction that affects the airways and breathing. In many cases, asthma is triggered by exposure to an allergen in the environment (allergy-induced asthma).
- Atopic dermatitis (eczema), sinusitis, and infections of the ears or lungs. Your risk of getting these conditions is higher if you have hay fever, a pet allergy or a mold allergy.
- Fungal complications of your sinuses or your lungs. You're at increased risk of getting these conditions, known as allergic fungal sinusitis and allergic bronchopulmonary aspergillosis, if you're allergic to mold.
What you can do
- Write down your family's history of allergy and asthma, including specific types of allergies, if you know them.
- List medications, vitamins and supplements you take.
- Ask if you should stop any medications before your appointment. For example, antihistamines can affect the results of an allergy skin test.
- Skin test. Your skin is pricked and exposed to small amounts of the proteins found in potential allergens. If you're allergic, you'll likely develop a raised bump (hive) at the test location on your skin. Allergy specialists usually are best equipped to perform and interpret allergy skin tests.
- Blood test. A blood test that's sometimes called the radioallergosorbent test (RAST) can measure your immune system's response to a specific allergen by measuring the amount of allergy-causing antibodies in your bloodstream, known as immunoglobulin E (IgE) antibodies. A blood sample is sent to a medical laboratory, where it can be tested for evidence of sensitivity to possible allergens.
Allergy treatments include:
- Allergen avoidance. Your doctor will help you take steps to identify and avoid your allergy triggers. This is generally the most important step in preventing allergic reactions and reducing symptoms.
- Medications to reduce symptoms. Depending on your allergy, allergy medications can help reduce your immune system reaction and ease symptoms. Medications can include over-the-counter or prescription medications in the form of oral medications, nasal sprays or eyedrops.
- Immunotherapy. For severe allergies or allergies not completely relieved by other treatment, your doctor may recommend allergen immunotherapy. This treatment involves a series of injections of purified allergen extracts, usually given over a period of a few years.
- Another form of immunotherapy is a tablet that's placed under the tongue (sublingual) until it dissolves. Sublingual drugs are used to treat some pollen allergies.
- Emergency epinephrine. If you have a severe allergy, your doctor may give you an emergency epinephrine shot to carry with you at all times. Given for severe allergic reactions, an epinephrine shot (EpiPen, Auvi-Q, others) can reduce symptoms until you get emergency treatment.
- Sinus congestion and hay fever symptoms. These symptoms often improve with saline nasal irrigation — rinsing out the sinuses with a salt and water solution. You can use a neti pot or a specially designed squeeze bottle to flush out thickened mucus and irritants from your nose.
- Use water that's distilled, sterile, previously boiled and cooled, or filtered using a filter with an absolute pore size of 1 micron or smaller to make up the irrigation solution. Prepare the saline solution with the appropriate water, using the mixture supplied by the neti pot or one you make.
- Be sure to rinse the irrigation device after each use with distilled, sterile, previously boiled and cooled, or filtered water and leave open to air dry.
- Household airborne allergy symptoms. Reduce your exposure to dust mites or pet dander by frequently washing bedding and stuffed toys in hot water, maintaining low humidity, regularly using a vacuum with a fine filter such as a high-efficiency particulate air (HEPA) filter and replacing carpeting with hard flooring.
- Mold allergy symptoms. Reduce moisture in damp areas, such as your bath and kitchen, by using ventilation fans and dehumidifiers. Fix leaks inside and outside your home.
- Avoid known triggers. Even if you're treating your allergy symptoms, try to avoid triggers. If, for instance, you're allergic to pollen, stay inside with windows and doors closed during periods when pollen is high. If you're allergic to dust mites, dust and vacuum and wash bedding often.
- Keep a diary. When trying to identify what causes or worsens your allergic symptoms, track your activities and what you eat, when symptoms occur and what seems to help. This may help you and your doctor identify triggers.